ChemSex and HIV/HCV co-infection
 There’s an online piece of information that might just help prevent the New Year from becoming a bad year.
There’s an online piece of information that might just help prevent the New Year from becoming a bad year.
For those who are into ChemSex and are not aware of the dangers that can be associated with it, have a read… and stay safe.
· 7% of gay men in the UK co-infected with HIV and hepatitis C (HCV).
· 84% of the 218 newly diagnosed HCV infections were in London in data published in 2011.
· Rate of liver scarring in HIV/HCV-co-infected has been found to occur 12 years sooner than in HCV-monoinfected patients.
· In England deaths from hepatitis C rose by over 300% from 1996-2010.
· Successful treatment of HCV in HIV/HCV-co-infected patients reduces chance of liver-related death.
 56 Dean Street continues to be at the forefront of raising awareness and tackling the most urgent health needs in the gay community with the launch of an informative discussion guide about ChemSex and HIV/HCV co-infection. Following over 500 conversations with MSM (men who have sex with men), the guide, which is endorsed by The Hepatitis C Trust, aims to educate healthcare workers across the UK about the activities, risk factors and terminology associated with ChemSex and to ensure they are armed with the necessary information to have effective conversations and encourage testing and treatment.
56 Dean Street continues to be at the forefront of raising awareness and tackling the most urgent health needs in the gay community with the launch of an informative discussion guide about ChemSex and HIV/HCV co-infection. Following over 500 conversations with MSM (men who have sex with men), the guide, which is endorsed by The Hepatitis C Trust, aims to educate healthcare workers across the UK about the activities, risk factors and terminology associated with ChemSex and to ensure they are armed with the necessary information to have effective conversations and encourage testing and treatment.
MSM are increasingly using recreational drugs such as GBL, GHB, meth and mephedrone during sexual activities, which enhance the experience and are associated with high risk of STIs. When these men present in clinics, often healthcare providers struggle to understand how to communicate appropriately with this group, thereby limiting the identification of exposure to risks or an existing infection. With 92% of the newly 218 diagnosed HCV infections in the UK in 2011 occurring among MSM who were HIV-positive, the time is now to address this public health situation.2
David Stuart, Substance Use Lead at 56 Dean Street said: “We are seeing more and more MSM presenting at the clinic following a weekend bender of ChemSex and highly-charged sexual activity. Worryingly, many MSM who are well informed and proactive about their HIV management are often less willing to accept HCV risks and tests. From our experience, by understanding the cultural and behavioural contexts of MSM and using terminology that they understand, risks can be assessed and we can ensure those needing testing or treatment are seen to. We hope the guide will be an invaluable resource for healthcare providers across the UK who may not be familiar with how best to communicate with these men, and that open conversations will help this tackle this trend.’
The increase in ChemSex and HIV/HCV co-infection is a result of several factors; the availability of recreational drugs, sexual activities organised online and through apps, often taking place in private homes rather than public sex venues. This makes the group not only hard-to-reach, but also difficult to understand exactly what activities are taking place and how to message public health initiatives. As such, sexual health clinics are the new front line in addressing these complex risks and harms, and staff in these clinics need tools to raise awareness and skills beyond their traditional remit.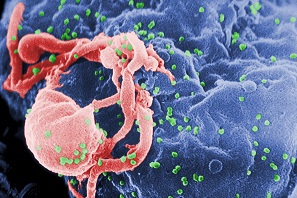
Charles Gore, CEO of The Hepatitis C Trust commented: “We are seeing a worrying increase in hepatitis C infection among men who are aware of the dangers of HIV/HCV co-infection and who are being treated for hepatitis C multiple times but who seem either unaware of the precise risks for contracting hepatitis C or are unable to mitigate those risks successfully. Tools like this guide therefore have a vital role in helping this well-informed and active community, with support from their HCP, identify and halt what can be a deadly combination of diseases.”
The primary goal is prevention of HIV/HCV co-infection, but it is also important for co-infected individuals to be tested and treated. Successful treatment of HCV in HIV/HCV-co-infected patients is associated with decreased liver-related mortality, as well as non-liver-related mortality, and AIDS progression. Early detection and diagnosis of HCV enables appropriate treatment to be provided for the best chance of the patient clearing the virus.
The ChemSex and hepatitis C: a discussion guide for HCPs can be downloaded by visiting 56 Dean Street’s website.

